One of the core transformations in healthcare in recent years has been a shift towards value-based care models, and a focus on preventive measures to reduce overall healthcare costs. As part of this shift, primary care practices are exploring innovative ways to improve patient access to care and engage patients through ongoing “longitudinal” care – care that supports a population throughout their lifetime, rather than just during episodic time periods.
One effective strategy to support this is the integration of physical therapists (PTs) into advanced primary care practices, where PTs can help patients sooner in the care journey. In this blog post, we’ll discuss in detail how PTs, as longitudinal patient engagement experts, can best serve patient populations and utilize their unique skills by being incorporated into these multidisciplinary practices.
The changing healthcare landscape
More and more, healthcare providers are participating in Medicare and Medicaid-sponsored alternative payment models which incentivize providing “the right care at the right place at the right time.” Private payers are developing similar programs, focused on incentivizing and reimbursing care that avoids preventable inpatient spending and poor outcomes, and that encourages providers to engage their patients in managing their health through longitudinal patient-provider relationships and team-based care.
This shift is also driven by the growing understanding that high-value, easily accessible primary care is essential for improving population health and reducing healthcare costs. Trade associations and advocacy groups have been informing CMS’ evolving policies and innovation opportunities, and payment models like the Medicare Shared Savings Program have received meaningful updates over the last 2 years.
CMS is simultaneously investing more of the annual budget into incentives for primary care to provide team-based, whole-person care and for practices to evolve to support a new paradigm of patient care. From upfront funding opportunities, to new services and billing codes, to improved benchmarking – CMS expects the recent updates to get them closer to their goal of 100% of Medicare beneficiaries in an accountable care relationship with a provider responsible for the cost and quality of their care by 2030. This opens the door for other providers who excel at preventative and high-value, first-touch care to support primary care practices.
Physical therapists: cost-effective, longitudinal patient engagement experts
A hallmark skill of PTs is their expertise in patient engagement. The real opportunity in front of PTs is to use their skills in communicating and connecting with patients to provide both preventative and urgent care to populations, deepen trust over time, and expand access to care in new ways.
I would argue that the advanced primary care practice in substantial payer risk arrangements is successful when it can do these two primary things:
- Provide easy and quick access to the right care at the right time within the practice to address urgent needs
- Develop and maintain a long-term, trusted relationship with their patient population, which can entail:
- Outreach to patients for their Annual Wellness Visit and to ensure evidence-based preventative care is delivered
- Patient education and support to address individual health risks and recommended behavior changes
- Identifying chronic health conditions early, and working with patients as care partners as they become proficient in managing those conditions
- Creating simple, friendly, habitual ways for patients to communicate with the practice at any day and time
A physical therapist in a primary care practice is valuable for a number of reasons:
- As a trusted front-line provider on a physician’s primary care team
- Providing first-touch care when patients visit the primary care practice for musculoskeletal pain, weakness, dizziness, gait imbalances, and more
- For decanting patients most likely to need a PT rather than a physician
- For supporting components of the Annual Wellness Visit, by being directly referred patients after an AWV identifies the need
- Immediately addressing patient impairments identified by the physician when they see the patient first (ex: patient sees physician for a fever, receives medical care, and is referred directly to the PT secondary for a change in gait from prior interactions to address safety, balance, and develop a PT plan of care as needed)
- As experts in discharge planning, rehabilitation, and post-acute sites of care, working with practice navigators, acute care facilities, and post-acute facilities to support patients and care partners when a patient has an acute hospital stay
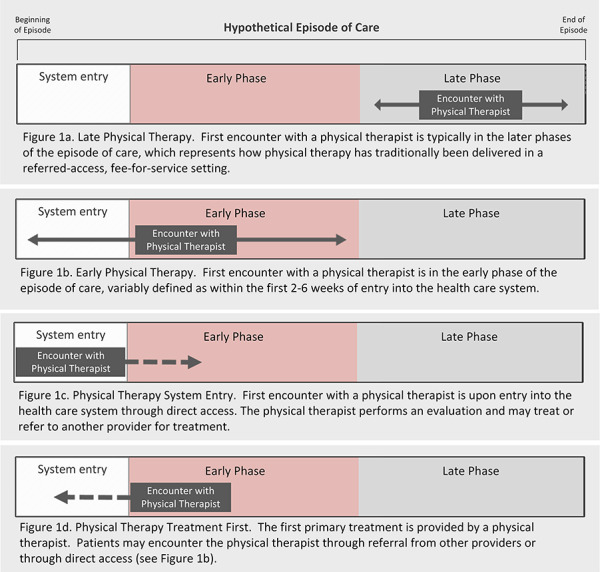
High-value care to patients means care that is both higher quality and lower cost. Along that line, there are financial advantages of early intervention and preventive care provided by PTs. A 2020 research article in the Journal of the American Physical Therapy Association includes this visual:
The authors explain that Figure 1d. is the “physical therapist treatment first” model – where patients are treated by a PT through a model that typically colocates physical therapy at sites of care in which patients are already seeking care, such as in primary care and in the emergency department. In this workflow, patients are immediately referred for treatment first by the PT.
By addressing musculoskeletal and other issues promptly, physical therapists are a direct solution to high-cost, low-value (and sometimes high-risk) care such as opioids, surgeries, unnecessary imaging and specialty physician visits, hospital and post-acute stays, and more.
Reducing access to care barriers
One of the challenges faced by primary care practices is improving patient access to care while optimizing resources. By adding physical therapists to their on-site care teams, these practices can enhance efficiency and effectiveness in the following ways:
- PTs can provide timely evaluations and treatments, allowing physicians, advanced practice nurses, and physician assistants to focus on their medical areas of expertise where they are uniquely licensed to practice.
- The presence of PTs within primary care practices also reduces the need for referrals to external providers, streamlining the patient’s journey through the healthcare system. Patients receive necessary interventions without unnecessary delays.
- The integration of PTs into interprofessional population health management within and outside the practice. PTs can add additional support and expertise in collaborating with others providing care to the patient outside the practice.
Interprofessional collaboration is sometimes just a buzzword. But in an evolving healthcare landscape, there are new reasons to care that each professional brings their unique expertise to the table. Physical therapists have often struggled to engage with physicians, as there have been no financial incentives to do so. But with primary care providers (PCPs) entering into outcomes-based risk arrangements, even interprofessional collaboration takes on new meaning as a financial opportunity. It’s an unavoidable truth – like almost all professions, incentives are driven by how money is earned.
Preventative and longitudinal care services and codes
Payers reimbursing for preventative care and screenings is a relatively new concept. Codes classified as “preventative” services do not have a copay and must be reimbursed as part of the Affordable Care Act policies.
One of the key services in this space is the Annual Wellness Visit (AWV). It is a critical component in risk-based programs because it gives the primary care team an opportunity to comprehensively evaluate a patient’s medical conditions and risks. It is also a place where annual and periodic screenings can be scheduled, a chance to enroll patients with chronic conditions in disease management programs, and a way to build trust with the members of the care team and their primary care providers.
A common screening performed during an AWV is a fall screening. It’s a quality measure for many payers and a standard practice during an AWV. For patients who score as a fall risk, there is no better professional to evaluate that patient than a PT on the primary care team. They are licensed to evaluate and treat and/or refer as needed. Right now, it’s common for a positive screening for falls to just be documented in the record, with nothing done to address this finding.
This year, CMS even finalized new codes so that care teams can evaluate and bill for “Social Determinants of Health Screening” twice per year. They can then connect beneficiaries to community resources and other services while being able to bill for “Community Health Integration (CHI).” They also added codes for “Principal Illness Navigation (PIN).” These CHI and PIN codes can be billed for services provided by non-licensed members of the primary care team, including community health workers.
They also finalized new codes for therapists specifically to provide “Caregiver Training.” There are codes for PTs, OTs, and STs to provide this service. This is essentially an invitation by CMS to reimagine the role of rehabilitation professionals as primary care team members. APTA members can watch it at no cost here (register for the November 2023 event and watch the recording).
Upstream/preventative care and downstream/urgent care
As previously noted, we can reduce spending and poor outcomes over time through long-term prevention and early detection strategies, longitudinal patient engagement, and improving access to care. All of these benefit from multi-pronged approaches.
By conducting and/or receiving referrals from screenings and assessments right within the practice, physical therapists can address potential issues and implement preventive strategies such as:
- Exercise programs
- Education on proper body mechanics
- Addressing balance disorders and progressive weakness from chronic conditions
- Lifestyle modifications.
This proactive approach can play a crucial role in ultimately improving patient outcomes and reducing healthcare costs.
On the other hand, PTs can also provide valuable support in downstream/urgent care. In situations where patients require immediate attention for acute injuries or exacerbations of chronic conditions, PTs can play a vital role in providing timely interventions.
Conclusion
The integration of physical therapists into advanced primary care practices offers numerous benefits for both patients and healthcare systems. As longitudinal patient engagement experts, PTs bring unique skills and perspectives that enhance the overall quality of care provided. By embracing the role of embedded PTs, advanced primary care practices can further enhance patient engagement, improve outcomes, and optimize resources.
It will be up to the PT community to learn about present and emerging advanced primary care incentive payment initiatives. Primary care medical providers are the “quarterbacks” of medical care around the world. While they have been historically underfunded in the United States, this is changing and momentum is growing.
PCPs can’t be successful on their own. As they apply for federal and state-based programs, they are also building the structure and strategies to achieve success through care transformation and team-based care.
The question is: Will physical therapists be part of the solution and cement a role in advanced primary care? It makes complete sense that this is a critical site of care for PTs to have the most impact and achieve greater professional satisfaction. All we have to do now is take action.
About the author:
Dana Prommel Strauss is a doctor of physical therapy and a public policy analyst specializing in value-based health care, home-based care, and Medicare payment systems and alternative payment models. She started a free newsletter, Timeless Autonomy, and writes about healthcare policy, news, and innovation in healthcare delivery. You can subscribe to her newsletter here.
Learn more: How can PTs explore this opportunity?
An increasingly popular alternative payment model solution is directing more of the total healthcare dollars prospectively to primary care practices. They then have the funding to transform how they care for a population. Payers directly incentivize them financially to prevent hospitalizations, unnecessary specialty care, and inadequate or delayed care of chronic conditions, among other things.
Payers are removing the incentive to provide a high-volume of care, and replacing that with the incentives to provide the ideal, evidence-based care, both upstream and downstream.
The first step for PTs is to learn more about advanced primary care payment methodologies and the difference between fee-for-service and risk-based primary care practice. To be willing to do that, PTs must first release old ideas about practice that is independent from physicians. Some resources to start you off:
- ACO REACH Model
- NASEM’s Report on Primary Care
- CMS Innovation Center’s Strategy to Support High-Quality Primary Care
- AJMC: Primary Care Transformation: A Team-Based Care Model
- Multi-association letter to CMS calling for a hybrid prospective payment model
- Advanced Primary Care defined by the Primary Care Collaborative
Because here’s the bottom line: Both PCPs and PTs have expertise in primary preventative care, longitudinal care, team-based care, collaboration with medical specialists, and more. By directly collaborating on advanced primary care teams, you can collectively quarterback each person’s care for whom they are accountable. The key opportunity is healthcare reform centered on high-quality patient outcomes and lowering the total cost of care.
To help summarize:
- Primary care physicians and NPPs are not the best professionals to address most musculoskeletal pain, weakness, balance disorders, etc. (or not in a vacuum).
- Physical therapists are not the best professionals to address medical illness (or not in a vacuum).
- Working together, they can improve access to primary care while patients are directed right to the providers most likely to address their needs. And when both the PCP and the PT should both see a patient in one visit, both are right there to do that.
Once PTs understand the structure and payment methodologies for advanced primary care practices, the next step is research to identify participating practices and organizations and then demonstrating how a PT embedded in the practice can help them achieve their care transformation and financial goals.
It’s a new idea to digest, but hopefully this plants a few seeds. Bookmark this article and come back to it when the seed is fertilized!